Revolutionizing RCM: Unleash Your Practice’s Full Financial Potential
Achieve under 3% denial rates and 95% first-pass approvals.*

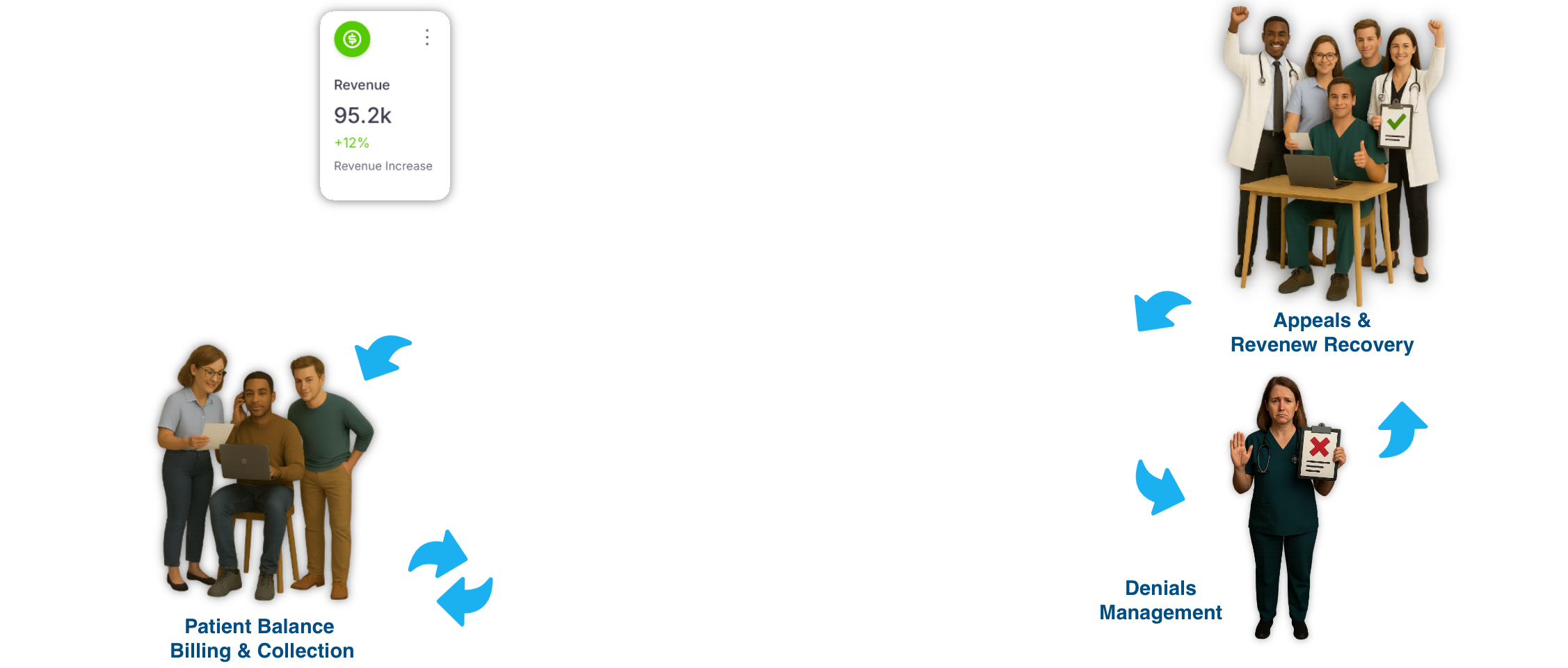
CORDINA™ streamlines processes across four key areas using automation, AI, and real-time analytics, with human supervision integrated throughout the entire process as needed. This approach enables healthcare organizations to accelerate reimbursements, reduce administrative burdens, and significantly enhance financial performance.
Front-End Accuracy
Ensure that the initial stages of the revenue cycle—patient intake, insurance verification, and pre-authorization—are done with precision. These foundational processes directly affect claim accuracy and reimbursement timelines.
Mid-Cycle Controls
Control critical stages of claims creation, coding, and submission. Ensuring these steps are handled with the highest level of accuracy and compliance is crucial for first-pass resolution (FPR) and reducing rework.
Back-End Rigor
Ensure that once claims are submitted, they are handled efficiently through remittance matching, denial management, and patient billing. This phase is essential to ensure that every dollar earned is collected.
Analytics & Compliance
Provide continuous oversight and intelligence across the revenue cycle, allowing organizations to stay compliant, optimize operations, and improve overall financial performance.
onboarding experience tailored to your workflow.
Browse through these FAQs to find answers to commonly asked questions.
Any question or remark? Just write us a message.